What is The Mechanism of Action of Ibogaine?
Ibogaine’s mechanism of action is one of the most complex topics in addiction medicine, involving multiple brain systems that scientists are still working to understand. This deep dive is designed for researchers, clinicians, and anyone curious about how this controversial compound affects the brain and potentially treats addiction.
Ibogaine doesn’t work through a single pathway like most drugs. Instead, it hits multiple neurotransmitter systems at once, creating a web of interactions that make it both fascinating and challenging to study. Its active metabolite, noribogaine, adds another layer of complexity with its own distinct effects that can last for days or weeks.
We’ll break down how ibogaine modulates dopamine systems in addiction-related brain regions and explore the specific receptor interactions that drive its anti-addiction properties. You’ll also discover how noribogaine’s unique pharmacological profile contributes to ibogaine’s long-term therapeutic effects, and why different receptor combinations may explain why the compound works differently for opioid addiction versus cocaine or alcohol dependence.
Multiple Neurotransmitter System Interactions
Serotonergic Receptor Activation and Modulation
The ibogaine mechanism of action demonstrates complex interactions with serotonergic systems, despite being a cyclized derivative of serotonin that shows relatively low affinity for most serotonin receptors. Research using rodent drug discrimination studies reveals that ibogaine partially substitutes for serotonergic psychedelics LSD and DOM, an interaction that can be blocked by the serotonin 5-HT2 receptor antagonist pizotifen.
The 5-HT2A and 5-HT2C receptors appear to be the primary serotonergic targets involved in ibogaine’s subjective effects. The preferential serotonin 5-HT2C receptor agonists MK-212 and mCPP partially substitute for ibogaine, and this substitution can be blocked by the serotonin 5-HT2 receptor antagonist metergoline. Additionally, the serotonin releasing agent fenfluramine, which acts as a potent serotonin 5-HT2 receptor agonist, also partially substitutes for ibogaine.
Interestingly, while serotonin 5-HT2A receptor signaling contributes to ibogaine’s effects, neither ibogaine nor its major active metabolite noribogaine appear to act as direct serotonin 5-HT2A receptor agonists. Furthermore, the serotonin 5-HT1A and 5-HT3 receptors do not appear to be involved in ibogaine’s mechanism of action.
Opioid Receptor Binding and Effects
Ibogaine neurotransmitter effects include significant interactions with multiple opioid receptor subtypes. The compound demonstrates binding affinity for mu, delta, and kappa opioid receptors, contributing to its complex pharmacological profile. These opioid receptor interactions are particularly relevant to understanding ibogaine’s anti-addiction properties.
The noribogaine metabolite shows distinct opioid receptor activity, acting as a moderate κ-opioid receptor agonist and a weak μ-opioid receptor agonist or weak partial agonist. This κ-opioid receptor activity may contribute significantly to the psychoactive effects attributed to ibogaine ingestion, similar to how salvinorin A from Salvia divinorum produces strong hallucinogenic properties through highly selective κ-opioid agonism.
Animal studies suggest that the μ- and/or κ-opioid receptors may be involved in the subjective effects of ibogaine, making these interactions crucial for understanding the therapeutic mechanisms underlying ibogaine treatment.
Sigma Receptor Interactions
The sigma σ2 receptor appears to be involved in ibogaine’s subjective effects based on animal studies, while the sigma σ1 receptor does not appear to contribute to the compound’s mechanism of action. This selective sigma receptor interaction adds another layer to ibogaine’s complex pharmacological profile.
These sigma receptor interactions may contribute to the unique therapeutic properties of ibogaine, though the specific mechanisms through which sigma σ2 receptor activation influences the compound’s anti-addictive effects require further investigation.
NMDA Receptor Involvement
Ibogaine demonstrates interactions with N-methyl-D-aspartic acid (NMDA) associated ion channels, as determined by the inhibition of [³H]MK-801 binding. However, animal studies indicate that NMDA receptors do not appear to be directly involved in ibogaine’s subjective effects, despite this binding interaction.
The compound also interacts with sodium ion channels, as evidenced by the inhibition of [³H]batrachotoxin A 20-alpha-benzoate binding. These ion channel interactions contribute to ibogaine’s broad spectrum of neurological activity and may play a role in its overall therapeutic profile, even if they don’t directly mediate the primary psychoactive effects.
This complex pattern of ibogaine receptor interactions across multiple neurotransmitter systems suggests that the compound’s putative anti-addictive activity results from multiple mechanisms of action working simultaneously rather than through a single primary target.
Noribogaine Metabolite’s Distinct Pharmacological Profile
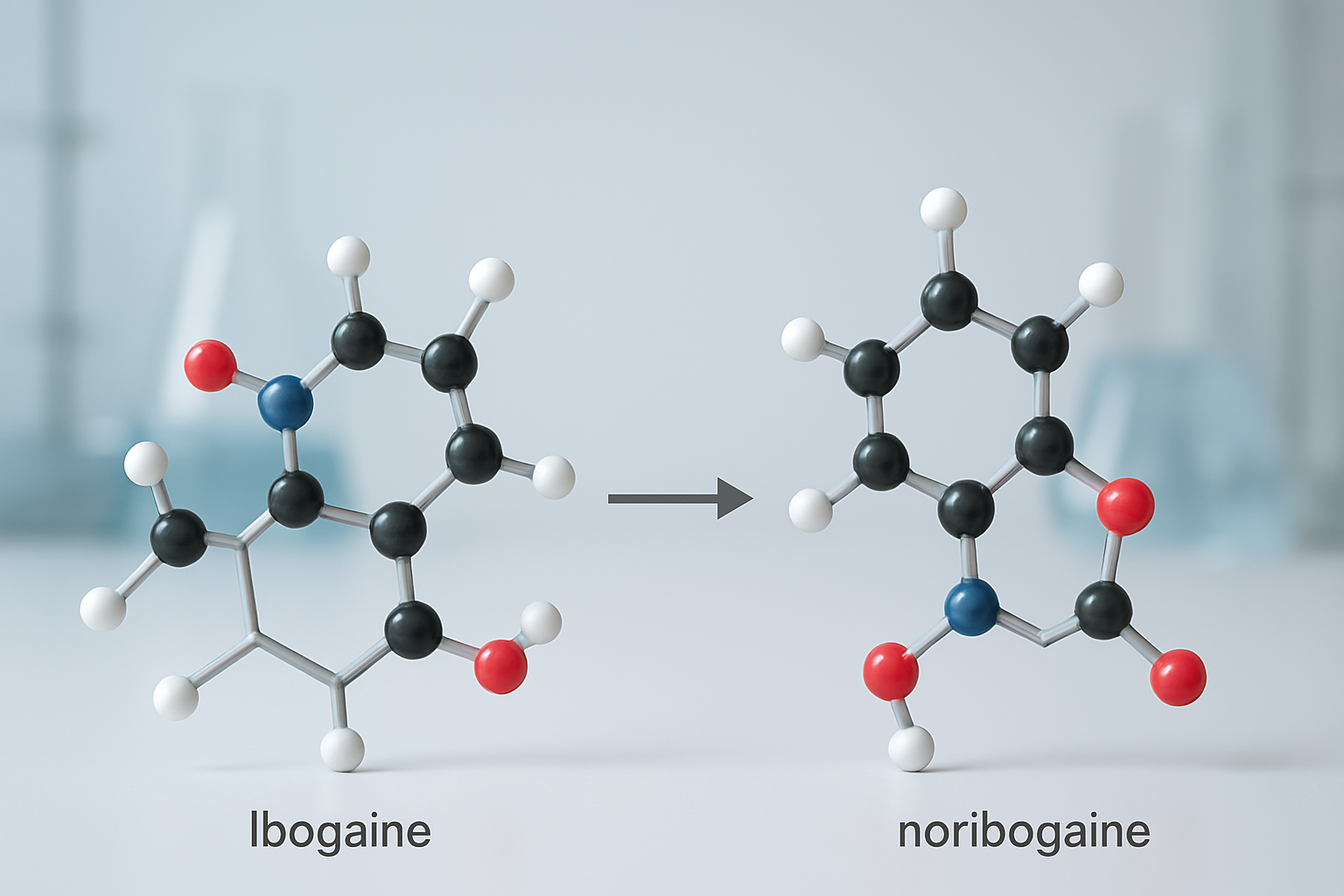
Serotonin Reuptake Inhibition Properties
Noribogaine demonstrates significantly more potent serotonin reuptake inhibition properties compared to its parent compound ibogaine. The metabolite exhibits an IC50 of 0.18 μM for serotonin reuptake inhibition, which is substantially more powerful than ibogaine’s IC50 of 3.85 μM. This enhanced potency means noribogaine increases extracellular serotonin levels more effectively than ibogaine itself.
The mechanism involves noribogaine binding to the central binding site of the serotonin transporter (SERT), with binding affinity values ranging from 41 nM (Ki) to 280-326 nM (IC50). The closure of the extracellular gate depends on transmembrane helices 1b and 6a movements, while intracellular gate opening involves hinge-like movement of TM1a and partial unwinding of TM5, allowing substrate and ions to cross the membrane through permeation.
This increased serotonin transmission associates with elevated brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF) expression and signaling. Both ibogaine and noribogaine can produce antidepressant-like effects in animal models, such as in the forced swim test in rats. Importantly, noribogaine’s affinity for 5-HT receptors in the brain is ten times higher than that of ibogaine, contributing to its distinct pharmacological profile and therapeutic potential.
Kappa-Opioid Receptor Agonist Activity
Noribogaine has been determined to act as a biased agonist of the κ-opioid receptor (KOR), representing one of its most potent pharmacological actions. The metabolite activates the G protein (GDP-GTP exchange) signaling pathway with 75% the efficacy of dynorphin A, with an EC50 value of 9 μM. However, noribogaine demonstrates only 12% efficacy at activating the β-arrestin pathway compared to full agonists.
This biased receptor activity is particularly significant because the β-arrestin signaling pathway is hypothesized to be responsible for the anxiogenic, dysphoric, or anhedonic effects typically associated with KOR activation. With an IC50 value of 1 μM, noribogaine can be regarded as an antagonist of the β-arrestin pathway. This attenuation of β-arrestin signaling may explain the absence of aversive effects while retaining analgesic and anti-addictive properties.
The binding affinity data shows noribogaine has a Ki value of 720 nM for KOR, with EC50 values ranging from 110-8,749 nM and maximal efficacy (Emax) between 13-85%. This biased KOR activity makes noribogaine stand out from other iboga alkaloids like ibogaine and 18-methoxycoronaridine (18-MC), positioning it among atypical or biased KOR agonists alongside compounds like RB-64, 6′-GNTI, herkinorin, and nalfurafine.
Role in Mediating Stimulus Properties
The role of noribogaine in mediating stimulus properties is supported by experimental observations from in vitro binding assays and animal pharmacology studies. These studies have identified biological activities for noribogaine that are relevant to consider regarding the overall therapeutic benefits and adverse off-target effects associated with oral ibogaine administrations.
Noribogaine demonstrates complex pharmacological properties that contribute to its role in mediating therapeutic effects. The metabolite shows high brain penetration in rodents due to its highly lipophilic nature, with an elimination half-life of 24 to 50 hours. This extended half-life suggests sustained activity that could contribute to ibogaine’s prolonged therapeutic effects.
Unlike ibogaine, noribogaine does not bind to the sigma σ2 receptor, indicating distinct pharmacological selectivity. The metabolite acts as a weak NMDA receptor antagonist and binds to opioid receptors, with greater affinity for each of the opioid receptors than ibogaine itself. Additionally, noribogaine has been reported as a low-efficacy serotonin releasing agent, though findings are conflicting and other studies suggest it may be inactive as a serotonin releasing agent.
The metabolite’s ability to modulate intracellular signaling linked to opioid receptors and potentiation of opioid-induced inhibition of adenylyl cyclase further contributes to its complex stimulus properties. Importantly, while ibogaine and structurally related compounds like harmaline are tremorigenic, noribogaine is not or is much less so, indicating a more favorable side effect profile.
Anti-Addictive Mechanisms for Different Substances
Morphine and Opioid Addiction Intervention
Ibogaine demonstrates significant efficacy in reducing morphine self-administration through its complex neurotransmitter interactions. Preclinical studies show that both ibogaine and its active metabolite noribogaine can decrease morphine self-administration for several days in laboratory animals. The anti-addictive mechanisms involve ibogaine’s binding affinity for kappa-opioid receptors and N-methyl-D-aspartate (NMDA) receptors, which appear to be crucial for its effects on opioid dependency.
When administered 19 hours prior, ibogaine pretreatment blocks morphine-induced dopamine release in the nucleus accumbens and prevents morphine-induced locomotor hyperactivity. The kappa agonist and NMDA antagonist actions contribute significantly to ibogaine’s effectiveness against opioid self-administration. These effects are supported by studies showing that kappa agonists like U50,488 and NMDA antagonists such as MK-801 can mimic several of ibogaine’s anti-opioid effects. Additionally, noribogaine’s weak or partial mu-opioid receptor agonist activity may help reduce withdrawal symptoms while contributing to the overall anti-addictive profile.
Cocaine and Stimulant Self-Administration Reduction
The ibogaine mechanism of action against stimulant addiction involves distinct pharmacological pathways compared to opioid intervention. Research demonstrates that ibogaine can decrease cocaine self-administration for several days, with effects mediated primarily through kappa-opioid receptor agonism and NMDA receptor antagonism. Interestingly, while ibogaine blocks morphine-induced effects, it actually enhances the dopamine-releasing effects of stimulants like cocaine and amphetamine when given as pretreatment.
Both ibogaine and noribogaine acutely decrease extracellular dopamine levels in the nucleus accumbens, which may contribute to their anti-addictive properties against stimulants. The therapeutic effects appear to result from the modulation of dopamine system activity rather than complete blockade, allowing for normalization of reward pathways without complete dopamine suppression.
Alcohol Intake Modulation Through Serotonergic Pathways
For alcohol addiction intervention, ibogaine’s anti-addictive mechanisms appear to operate primarily through serotonergic pathways rather than the opioid or dopaminergic mechanisms involved in other substances. Both ibogaine and noribogaine bind to serotonin uptake sites, with noribogaine functioning as a serotonin reuptake inhibitor. This serotonergic action is believed to be more important for ibogaine-induced decreases in alcohol intake compared to the kappa-opioid and NMDA receptor interactions that dominate its effects on opioids and stimulants.
The duration of alcohol intake reduction appears to be shorter-lasting compared to the effects observed with opioids and stimulants, suggesting that different receptor combinations and mechanisms may be responsible for ibogaine’s interactions with different drugs of abuse.
Nicotine Preference Reduction via Receptor Antagonism
Ibogaine’s effectiveness against nicotine addiction operates through a distinct nicotinic receptor antagonist mechanism. The compound demonstrates binding affinity for nicotinic receptors, and this nicotinic antagonist action appears to mediate ibogaine-induced reduction of nicotine preferences in laboratory studies. Ibogaine pretreatment blocks nicotine-induced dopamine release, similar to its effects on morphine-induced dopamine release, but through different receptor mechanisms.
The anti-nicotine effects of ibogaine appear to be shorter-lasting compared to its effects on opioid and stimulant self-administration. This suggests that the nicotinic receptor antagonism, while effective, may require different dosing strategies or combination approaches for sustained therapeutic benefit. The specificity of ibogaine’s nicotinic receptor interactions demonstrates the compound’s ability to target multiple addiction pathways through distinct pharmacological mechanisms tailored to different substances of abuse.
Dopamine System Modulation in the Brain
Acute Dopamine Level Reduction in Nucleus Accumbens
Ibogaine demonstrates pronounced effects on dopamine modulation within the nucleus accumbens, a critical brain region associated with reward processing and addiction. When administered at high concentrations (200-400 μM) through direct perfusion, ibogaine produces immediate decreases in extracellular dopamine levels while simultaneously increasing metabolite concentrations in both the nucleus accumbens and striatum.
These acute changes occur within 1-3 hours of administration and represent direct pharmacological action at dopaminergic nerve terminals. The reduction in dopamine availability coincides with enhanced metabolic activity, as evidenced by increased levels of dopamine metabolites such as DOPAC (3,4-dihydroxyphenylacetic acid). This dual effect suggests that ibogaine not only reduces dopamine release but also accelerates its metabolism, creating a comprehensive suppression of dopaminergic activity in reward-related brain circuits.
The ibogaine brain effects extend beyond simple receptor blockade, involving complex alterations in dopamine homeostasis that may contribute to its anti-addictive properties. These acute dopaminergic changes occur at concentrations that mirror the effects observed with systemic administration, confirming that ibogaine acts directly within brain regions containing dopaminergic terminals rather than through indirect systemic mechanisms.
Morphine-Induced Dopamine Release Blockade
Research demonstrates that ibogaine interferes with morphine’s ability to stimulate dopamine release in key brain regions. This interaction represents a crucial component of ibogaine anti-addiction therapy mechanisms, as morphine typically enhances dopaminergic activity in the nucleus accumbens, contributing to its rewarding and addictive properties.
The blockade of morphine-induced dopamine release occurs through direct pharmacodynamic interactions at the level of dopaminergic nerve terminals. Previous studies referenced in the research indicate that ibogaine not only affects baseline dopamine levels but also modulates the response to opioids, creating a protective effect against morphine’s neurochemical actions.
This dopamine modulation extends to both acute and persistent timeframes, with ibogaine’s effects on morphine-induced changes lasting well beyond the initial administration period. The ability to block morphine’s dopaminergic effects while maintaining direct action at nerve terminals positions ibogaine as a unique therapeutic agent that can interrupt the neurochemical cascade underlying opioid addiction.
Enhanced Stimulant Effects Through Pretreatment
Contrary to its suppressive effects on baseline dopamine levels, ibogaine pretreatment paradoxically enhances the dopaminergic responses to stimulant drugs like D-amphetamine. When ibogaine is administered 19 hours prior to amphetamine exposure, it significantly potentiates amphetamine-induced dopamine release in the nucleus accumbens.
This enhancement occurs through both local and systemic mechanisms. Local administration of low-concentration ibogaine (10 μM) amplifies the effects of systemically administered D-amphetamine (1.25 mg/kg), while systemic ibogaine pretreatment enhances responses to locally applied amphetamine (1-10 μM). These bidirectional interactions demonstrate that ibogaine pharmacology involves complex pharmacodynamic mechanisms beyond simple metabolic interference.
The enhancement effect suggests that ibogaine’s therapeutic duration includes long-lasting changes in dopaminergic sensitivity that persist well after acute administration. This phenomenon indicates that ibogaine may prime the dopamine system for enhanced responsiveness to stimulants while simultaneously reducing baseline dopaminergic activity. Such complex modulation patterns may contribute to ibogaine’s unique profile as an anti-addictive agent, though the clinical relevance of stimulant enhancement requires further investigation to fully understand its implications for ibogaine treatment mechanisms.
Receptor-Specific Contributions to Therapeutic Outcomes
Kappa Agonist and NMDA Antagonist Effects on Drug Self-Administration
Previously explored mechanisms reveal how ibogaine’s complex pharmacological profile enables targeted interventions across different addiction pathways. The compound’s actions as a mild NMDA receptor antagonist and its modulation of glutamatergic signaling represent critical components of its anti-addictive properties. Through mild NMDA receptor antagonism and stabilization of mGluR2/3 activity, ibogaine reduces excessive glutamate release associated with hyperexcitability and persistent maladaptive behavioral patterns.
This glutamatergic modulation directly impacts drug self-administration behaviors by addressing the neurochemical imbalances that perpetuate addictive cycles. The stabilization of glutamate activity helps normalize the heightened neural excitability that characterizes chronic substance use, while the NMDA antagonist properties contribute to interrupting established neural pathways associated with drug-seeking behaviors. These receptor-specific actions work synergistically to reduce the compulsive nature of substance use across various addiction types.
Serotonergic Actions for Alcohol Treatment
Now that we have covered glutamatergic mechanisms, ibogaine’s serotonergic actions present another crucial dimension of its therapeutic profile. The compound’s influence on monoaminergic tone, particularly within serotonergic systems, contributes significantly to its effectiveness in treating alcohol use disorders. This modulation of serotonergic pathways helps address the mood and emotional dysregulation commonly associated with alcohol dependency.
The ibogaine mechanism of action includes comprehensive monoaminergic system modulation, which supports emotional recalibration necessary for sustained recovery from alcohol addiction. These serotonergic effects complement the compound’s other receptor interactions, creating a multi-target approach that addresses both the neurochemical and psychological aspects of alcohol use disorder.
Nicotinic Antagonist Properties for Smoking Cessation
With this understanding of ibogaine’s multi-receptor interactions, its nicotinic antagonist properties represent a specialized mechanism for addressing nicotine addiction. The compound’s ability to modulate dopamine transporters and influence neurotrophic factor expression, particularly glial cell line derived neurotrophic factor (GDNF), creates an environment conducive to breaking nicotine dependency patterns.
These nicotinic receptor interactions work in conjunction with ibogaine’s dopaminergic pathway modulation to disrupt the reward mechanisms that maintain smoking behaviors. The upregulation of neurotrophic factors such as GDNF promotes dopaminergic neuron survival within the ventral tegmental area and nucleus accumbens, regions critically involved in nicotine addiction. This neuroplastic support enables the brain to recalibrate its reward systems, positioning ibogaine as a potential transdiagnostic interventional tool that addresses the underlying neurobiological foundations of nicotine dependence through receptor-specific mechanisms.

Ibogaine’s complex mechanism of action demonstrates how a single compound can simultaneously target multiple neurotransmitter systems to produce profound therapeutic effects. Through its interactions with serotonin, opioid, sigma, and NMDA receptors, along with the distinct pharmacological contributions of its metabolite noribogaine, ibogaine offers a unique approach to addiction treatment. The drug’s ability to modulate dopamine release in the nucleus accumbens while providing different receptor-specific actions for various substances of abuse highlights its versatility as a therapeutic agent.
The long-lasting effects of ibogaine, potentially mediated through slow release from fat tissue and conversion to noribogaine, suggest that understanding these mechanisms could lead to more targeted and effective treatments for addiction. As research continues to unravel the specific receptor combinations responsible for ibogaine’s anti-addictive properties across different substances, this knowledge may pave the way for developing safer, more selective therapeutic interventions that harness the most beneficial aspects of ibogaine’s complex pharmacological profile.
