What Is Ibogaine, and What Is It Used For?

Ibogaine is a powerful psychoactive compound extracted from an African plant that’s gaining serious attention as a breakthrough treatment for addiction and brain injuries. This naturally occurring alkaloid has been used for centuries in traditional healing ceremonies, but modern medical research is now uncovering its remarkable potential to treat conditions that have stumped doctors for decades.
This comprehensive guide is for anyone curious about ibogaine treatment – whether you’re struggling with addiction, dealing with traumatic brain injury, or simply want to understand this emerging psychedelic medicine. We’ll also cover essential information for healthcare professionals and family members seeking alternative treatment options.
We’ll explore how ibogaine works in your brain by targeting multiple neurotransmitter systems, examine the proven medical applications for addiction treatment that are showing incredible success rates, and dive into the groundbreaking research on ibogaine for PTSD and traumatic brain injury treatment. You’ll also learn about the safety considerations and current legal status that affects treatment access worldwide.
Understanding Ibogaine’s Origins and Properties

Natural source from African iboga plant and traditional spiritual uses
Ibogaine originates from the root bark of Tabernanthe iboga, a shrub native to West Central Africa and member of the Apocynaceae family that thrives in the tropical forests of the region. The psychoactive properties of the iboga tree root bark were first discovered by forager tribes in Central Africa, who subsequently passed this knowledge to the Bwiti tribe of Gabon. This traditional knowledge was first documented in the 19th century for its spiritual applications.
Within African spiritual and shamanic practices, iboga has played a central role, most notably in the Bwiti religion where it serves as a sacred sacrament. Traditional practitioners use iboga-containing preparations in ritualistic ceremonies designed to facilitate contact with spiritual ancestors and support personal quests for knowledge and inner power. The plant material is typically prepared as shredded bark powder from T. iboga for consumption during these ceremonial contexts.
The traditional use of ibogaine demonstrates cultural sensitivity requirements, as this substance has been employed in ritual and medicinal contexts throughout West Africa for generations, representing deep-rooted indigenous knowledge systems that predate Western scientific investigation.
Chemical classification as psychoactive indole alkaloid with hallucinogenic effects
Ibogaine is classified as a psychoactive indole alkaloid, specifically a substituted tryptamine with the chemical formula C₂₀H₂₆N₂O and a molecular weight of 310.441 g/mol. The compound’s chemical structure was first elucidated in 1958 through X-ray diffraction analysis, with its melting point established at 152-153°C. Ibogaine contains two separate chiral centers, meaning four different stereoisomers exist, though these are difficult to resolve during synthesis.
As a hallucinogenic compound, ibogaine exhibits complex psychoactive effects that induce experiences qualitatively different from ordinary consciousness, often compared to trances, meditations, and dreams. The substance is further classified as having oneirogenic properties, meaning it produces dream-like states of consciousness. At therapeutic doses ranging from 1,000-1,500 mg orally, ibogaine produces pronounced hallucinogenic effects with a duration of 18-36 hours, though lower doses of 200-400 mg remain psychoactive, and very low doses of 8-30 mg have been reported to produce stimulant effects.
The psychoactive experience follows a characteristic three-phase progression: the acute visionary phase lasting 4-8 hours featuring dream-like consciousness with vivid visual imagery; the evaluative introspective phase spanning 8-20 hours where sensation normalizes but side effects persist; and residual stimulation lasting 24-72+ hours characterized by mood changes including potential depression and mania.
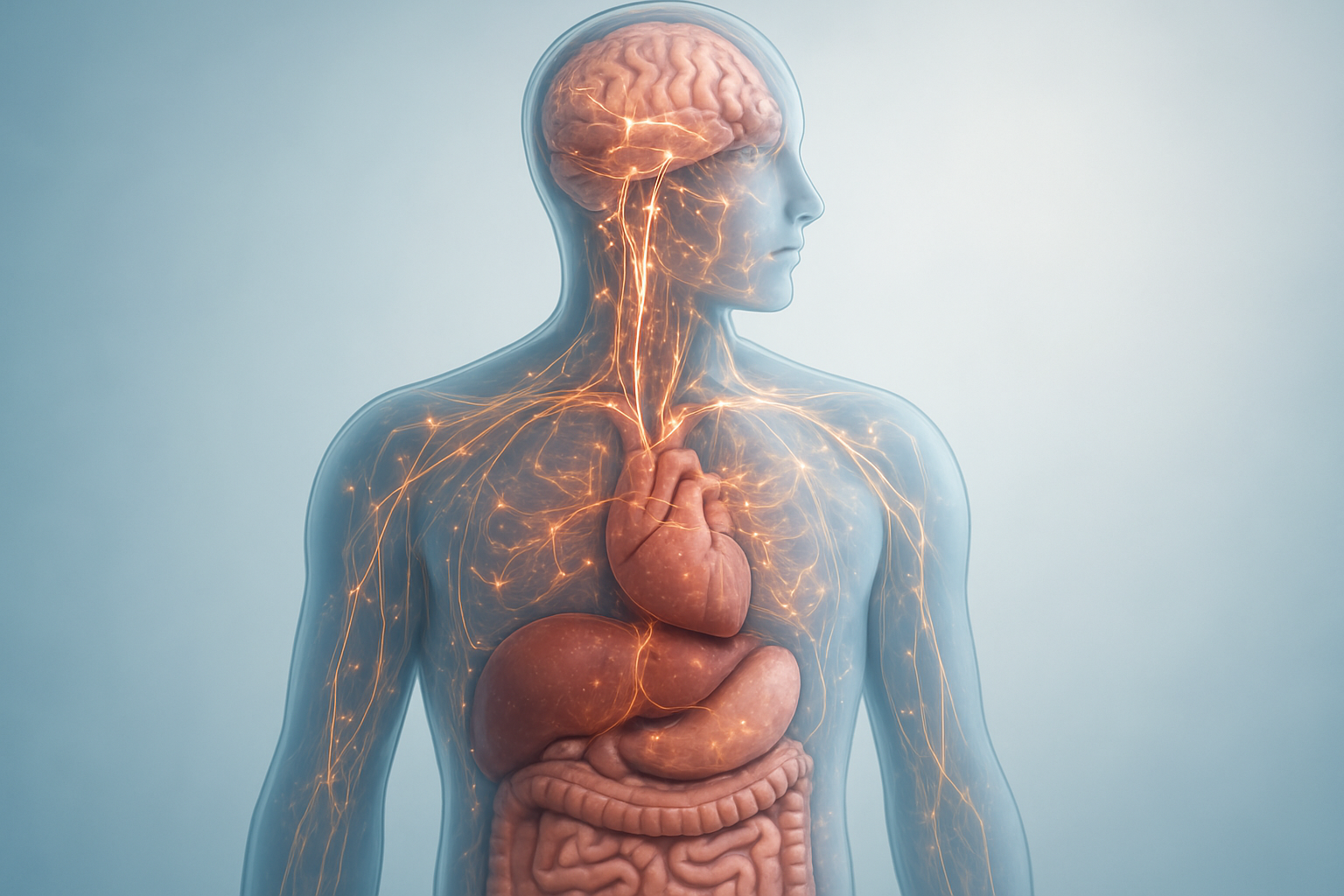
Complex pharmacology affecting multiple neurotransmitter systems
Ibogaine demonstrates remarkably complex pharmacological actions, interacting simultaneously with multiple neurotransmitter systems throughout the central nervous system. The compound exhibits high binding affinity for numerous receptor types, including μ-opioid, κ-opioid, and δ-opioid receptors, where it shows particular potency as a selective agonist at κ-opioid and sigma-2 receptors.
At glutamatergic synapses, ibogaine functions as a noncompetitive antagonist at NMDA receptor-coupled ion channels with a Ki of approximately 1 μM, competitively inhibiting [³H]MK-801 binding. The compound also acts as a noncompetitive antagonist at α3β4 nicotinic acetylcholine receptors, contributing to its complex neurological effects.
Within the serotonergic system, ibogaine demonstrates agonist activity at serotonin 5-HT2A and 5-HT2C receptors, while also inhibiting the serotonin transporter (SERT) with a Ki of approximately 10 μM. The compound’s interaction with dopaminergic transmission occurs through binding to dopamine transporters (DAT), where it inhibits dopamine uptake with a Ki of 1.5-4 μM and affects vesicular monoamine transporters.
Following oral administration, ibogaine undergoes metabolism by cytochrome P450 2D6 (CYP2D6) to produce noribogaine, a major active metabolite that exhibits distinct pharmacological properties. Noribogaine demonstrates greater potency as a serotonin reuptake inhibitor compared to its parent compound, with tenfold higher affinity for serotonin receptors and full agonist effects at moderate κ-opioid and weak μ-opioid receptors.
Both ibogaine and noribogaine are highly lipophilic compounds that accumulate in adipose tissue at concentrations 100 times higher than plasma and 30 times higher than brain tissue, contributing to the substance’s prolonged duration of action. The elimination half-life differs significantly between compounds, with ibogaine lasting approximately 7 hours while noribogaine persists for 24-50 hours, explaining the extended therapeutic effects observed clinically.
How Ibogaine Works in Your Body
Interaction with opioid, serotonin, sigma, and NMDA receptors
Now that we understand ibogaine’s origins, let’s explore how this complex alkaloid functions within your body at the molecular level. Ibogaine demonstrates remarkably complex pharmacology by affecting multiple neurotransmitter systems simultaneously, which distinguishes it from conventional medications that typically target single pathways.
The drug’s therapeutic effects appear to stem from its interactions with several key receptor systems. Research indicates that ibogaine’s subjective effects primarily involve serotonin 5-HT2A and 5-HT2C receptors, sigma σ2 receptors, and both μ-opioid and κ-opioid receptors. This multi-target approach creates a unique pharmacological profile that may explain ibogaine’s effectiveness in ibogaine addiction therapy.
Interestingly, while ibogaine is structurally derived from serotonin, it shows relatively low direct affinity for serotonin receptors. Instead, studies reveal that ibogaine partially substitutes for serotonergic psychedelics like LSD in laboratory settings, suggesting indirect serotonergic activity. However, unlike traditional psychedelics, ibogaine doesn’t appear to act primarily as a serotonin 5-HT2A receptor agonist, indicating a more complex mechanism of action.
The compound also interacts with NMDA-associated ion channels and sodium channels, contributing to its broad spectrum of neurological effects. Additionally, ibogaine affects dopamine and norepinephrine uptake sites, which may contribute to its anti-addictive properties.
Active metabolite noribogaine and its extended duration effects
With this multi-receptor activity in mind, the transformation of ibogaine into its primary metabolite noribogaine represents a crucial aspect of the ibogaine treatment experience. Noribogaine emerges as potentially more significant than the parent compound in mediating therapeutic effects, demonstrating similar discriminative properties while only partially substituting for ibogaine in research studies.
Noribogaine exhibits distinct pharmacological characteristics that extend the treatment’s duration. It functions most potently as a serotonin reuptake inhibitor, while also acting as a moderate κ-opioid receptor agonist and a weak μ-opioid receptor agonist or partial agonist. This metabolite proves more potent than ibogaine itself in laboratory discrimination assays, suggesting it may be primarily responsible for the sustained therapeutic effects observed in clinical settings.
The extended half-life of noribogaine means its effects can persist for days or even weeks after the initial ibogaine administration, providing a prolonged therapeutic window that may be crucial for addiction recovery and neuroplasticity changes.
Three-phase experience from visionary to introspective to residual stimulation
Understanding these receptor interactions helps explain the characteristic three-phase progression that defines the ibogaine treatment experience. The initial visionary phase typically involves intense hallucinogenic effects, likely mediated by the complex interplay between serotonin receptors, sigma receptors, and the compound’s unique binding profile across multiple neurotransmitter systems.
The second introspective phase represents a transition where patients often report deep psychological insights and emotional processing. During this period, the balance shifts toward noribogaine’s effects as the parent compound metabolizes, creating conditions conducive to therapeutic reflection and trauma processing.
The final residual stimulation phase can last for days, characterized by mild stimulant-like effects as noribogaine continues to influence serotonin reuptake and opioid receptor systems. This extended period may provide crucial neuroplastic changes that support long-term recovery outcomes in addiction treatment alternatives.
This three-phase progression reflects the dynamic interplay between ibogaine and noribogaine’s distinct receptor profiles, creating a comprehensive therapeutic experience that addresses both acute psychological processing and sustained neurochemical changes.
Breakthrough Treatment for Traumatic Brain Injury

Dramatic improvements in veterans with TBI-related symptoms
Research has revealed that ibogaine treatment may represent a groundbreaking approach for veterans suffering from traumatic brain injury (TBI) symptoms. A prospective study investigating the safety and efficacy of ibogaine-based therapy in Special Operations Veterans (SOVs) with histories of TBI and repeated blast/combat exposures showed remarkable improvements in disability symptoms with no serious adverse effects.
This emerging evidence suggests that ibogaine could be the first single treatment capable of improving chronic disability specifically related to repeated TBI from combat and blast exposures. Veterans who have endured the invisible wounds of war are increasingly seeking alternative therapies like ibogaine when traditional treatments fall short. The study’s findings indicate that this plant-based medicine may offer new hope for those struggling with persistent TBI-related complications.
The neurobiological mechanisms underlying these improvements appear linked to ibogaine’s ability to increase transcription of neurotrophic factors, including brain-derived neurotrophic factor and glial cell line-derived neurotrophic factor. Additionally, the compound increases cortical neuron dendritic arbor complexity, which may contribute to enhanced neural recovery and function in TBI patients.
Significant reduction in PTSD, anxiety, and depression symptoms
Beyond TBI-specific improvements, ibogaine treatment has demonstrated significant psychiatric benefits for veterans dealing with co-occurring mental health conditions. The research shows remarkable reductions in PTSD symptoms, anxiety, and depression among treated veterans, addressing the complex web of psychological challenges that often accompany traumatic brain injuries.
Veterans participating in ibogaine therapy have reported profound shifts in their mental health status following treatment. One veteran described how the experience helped address moral injury and trauma-related flashbacks that had persisted for years after deployment. The treatment appears particularly effective for veterans who have struggled with traditional psychiatric interventions or have reached crisis points in their mental health journey.
The psychiatric improvements observed extend beyond immediate symptom relief. Veterans report sustained benefits in mood regulation and emotional processing, suggesting that ibogaine’s effects on brain chemistry may create lasting positive changes rather than temporary symptomatic relief. This is particularly significant given that many veterans with TBI also struggle with treatment-resistant forms of PTSD and depression.
Enhanced cognitive function and daily life functioning
The cognitive benefits of ibogaine treatment for veterans with TBI represent one of the most promising aspects of this therapeutic approach. Studies have documented improvements in overall cognitive function that translate directly into enhanced daily life functioning for treated veterans.
Veterans report significant improvements in their ability to manage day-to-day activities, maintain relationships, and engage meaningfully with their communities following ibogaine treatment. These functional improvements appear to stem from the compound’s neuroplastic effects on brain tissue damaged by blast injuries and repeated trauma exposures.
The enhancement in cognitive function encompasses multiple domains, including improved memory processing, better emotional regulation, and enhanced decision-making capabilities. Veterans describe feeling more mentally clear and capable of engaging with life’s challenges without the cognitive fog that often accompanies TBI.
These improvements in daily functioning represent a critical breakthrough for veterans who have struggled with chronic disability related to their combat injuries. The ability to regain cognitive clarity and functional independence offers hope for thousands of veterans currently living with the long-term consequences of traumatic brain injury.
Safety Considerations and Risk Management

Serious Cardiovascular Risks Including Long QT Syndrome
Ibogaine poses significant cardiovascular risks that have been directly linked to multiple fatalities. The most concerning cardiac effect is QT interval prolongation, which can lead to potentially fatal arrhythmias. Case reports demonstrate QTc intervals reaching dangerous levels of 588 ms within hours of ibogaine administration, significantly exceeding the normal range of 450 ms.
The mechanism behind these cardiovascular complications involves ibogaine’s inhibition of human Ether-à-go-go-Related Gene (hERG) channels, which play a crucial role in cardiac repolarization. This interference with normal electrical conduction can trigger:
-
Torsade de pointes – A specific type of ventricular tachycardia
-
Ventricular fibrillation – Leading to cardiac arrest
-
Asystole – Complete cessation of heart rhythm
-
Sudden cardiac death – Often occurring within 72 hours of use
What makes ibogaine particularly dangerous is its unpredictable nature. Fatal cardiac events have occurred not only with high therapeutic doses but also with relatively small amounts – some fatalities involved less than half the recommended treatment dose of 20-30 mg/kg body weight. The drug’s highly lipophilic properties mean it’s stored in brain and adipose tissue, creating prolonged exposure even after initial administration.
Required Medical Supervision and Heart Protection Protocols
Given the documented cardiovascular risks, any ibogaine treatment requires comprehensive cardiac monitoring and emergency preparedness. Essential safety protocols must include:
Pre-treatment Cardiac Assessment:
-
Complete cardiovascular evaluation including family history screening
-
12-lead electrocardiogram to establish baseline QT interval
-
Echocardiogram to assess structural heart disease
-
Electrolyte panel focusing on potassium, magnesium, and calcium levels
Continuous Monitoring During Treatment:
-
Real-time cardiac telemetry for arrhythmia detection
-
Serial ECGs to track QT interval changes
-
Blood pressure and heart rate monitoring
-
Immediate access to advanced cardiac life support (ACLS)
Emergency Response Capabilities:
-
On-site defibrillation equipment
-
Intravenous access for emergency medications
-
Trained medical personnel experienced in cardiac emergencies
-
Protocols for managing torsade de pointes and ventricular arrhythmias
The reference cases highlight that cardiac arrest can occur suddenly and without warning. In one documented fatality, a patient was found in asystole approximately 8 hours after ibogaine administration, emphasizing the need for extended monitoring periods beyond the acute treatment phase.
Potential Drug Interactions and Contraindications
Ibogaine’s complex pharmacological profile creates numerous opportunities for dangerous drug interactions. The compound affects multiple neurotransmitter systems including opioid, serotonin, muscarinic, and nicotinic receptors, significantly increasing the risk of adverse interactions.
Absolute Contraindications:
-
History of cardiac arrhythmias or congenital long QT syndrome
-
Structural heart disease including cardiomyopathy
-
Current use of QT-prolonging medications
-
Severe liver or kidney dysfunction
-
Active substance use, particularly opioids
High-Risk Medication Interactions:
-
Opioid combinations – Evidence suggests ibogaine potentiates opioid toxicity, creating life-threatening respiratory depression
-
Antiarrhythmic drugs – May compound QT prolongation effects
-
Psychiatric medications – Particularly those affecting serotonin or dopamine systems
-
Anticholinesterase inhibitors – Ibogaine already inhibits cholinesterase activity
The timing of drug cessation before ibogaine treatment is critical. Concurrent opioid use has been implicated in several fatalities, as the combination appears to enhance toxicity rather than providing the intended withdrawal relief. Medical supervision must include comprehensive drug screening and sufficient washout periods for potentially interacting substances.
Laboratory monitoring should track liver enzymes, as ibogaine can cause hepatotoxicity, and kidney function, given reports of elevated creatinine levels in overdose cases. The unpredictable nature of ibogaine’s effects means that even patients without obvious risk factors have experienced fatal complications, underscoring the importance of treating every case as high-risk.
Legal Status and Treatment Access

Schedule I Classification in the United States
Ibogaine faces the most restrictive legal status in the United States, where it is classified as a Schedule I controlled substance under federal law. This classification places ibogaine in the same category as substances considered to have high abuse potential with no accepted medical use. The federal prohibition makes it illegal to possess, distribute, manufacture, or import ibogaine throughout the United States.
The Schedule I designation significantly impacts both research and treatment access. Unlike prescription medications, ibogaine cannot be legally prescribed by physicians or administered in clinical settings. Possession of ibogaine can result in serious legal consequences, including fines, arrest, and imprisonment under federal drug laws.
Despite these restrictions, some states are exploring legislative pathways to facilitate research. New York introduced Senate Bill S1817 to support research into ibogaine for substance use disorders, while Texas proposed HB 3717 to direct funding toward FDA clinical trials. However, these initiatives remain in early stages and do not change the current federal prohibition.
Legal Treatment Options in Mexico and Canada
Mexico presents a dramatically different legal landscape for ibogaine treatment. The substance remains completely unregulated in Mexico, creating an environment where ibogaine therapy centers can operate without legal restrictions. This unscheduled status has established Mexico as a primary destination for individuals seeking ibogaine addiction therapy, particularly those traveling from countries where the treatment is prohibited.
Canadian regulations take a middle-ground approach through the Prescription Drug List classification established in 2017. While ibogaine is controlled and cannot be freely distributed, Health Canada’s Special Access Program provides a legal pathway for medical professionals to request ibogaine for specific patients. However, access through this program is rarely granted, reflecting Canada’s cautious stance toward the treatment.
The contrast between these neighboring countries illustrates how different regulatory approaches affect treatment accessibility. Mexico’s unrestricted environment allows for immediate access but with varying oversight standards, while Canada’s controlled system provides legal protection but limited practical access.
Growing Government Investment in Clinical Research
The legal status of ibogaine is evolving as government agencies increasingly recognize its therapeutic potential through official research initiatives. Several countries are moving beyond outright prohibition toward regulated research programs that could reshape future legal frameworks.
In the United States, despite the Schedule I classification, state-level legislation is emerging to support clinical research. The proposed bills in New York and Texas represent a shift toward evidence-based policy making, directing resources toward FDA-approved clinical trials rather than maintaining blanket prohibition.
International regulatory bodies are also reassessing ibogaine’s classification based on accumulating research data. Countries like Brazil have already transitioned from prohibition to prescription-based access, with São Paulo legalizing ibogaine for medical use in 2016 before expanding to other regions.
This growing government investment in clinical research suggests a potential pathway toward broader legal access. As safety protocols are established and efficacy data accumulates through official channels, the current patchwork of international regulations may evolve toward more standardized frameworks that balance therapeutic access with appropriate medical oversight.
The regulatory landscape continues shifting as authorities weigh the mounting evidence for ibogaine’s therapeutic benefits against historical safety concerns, potentially leading to more nuanced legal classifications in the coming years.
Future Development and Therapeutic Potential

Non-hallucinogenic analogues in development
With the growing interest in ibogaine treatment, researchers are actively developing non-hallucinogenic analogues that could provide therapeutic benefits without the intense psychoactive effects. These modified compounds aim to retain ibogaine’s addiction-fighting properties while reducing the risks associated with the hallucinogenic experience. The development of these analogues represents a crucial step toward making ibogaine-based treatments more accessible and safer for patients seeking addiction therapy alternatives.
The collaborative research efforts, such as those being undertaken by the Texas consortium, are exploring various approaches to modify ibogaine’s molecular structure. By isolating the specific mechanisms responsible for addiction treatment while minimizing psychoactive components, scientists hope to create compounds that can be administered in standard clinical settings without requiring the intensive monitoring currently necessary for traditional ibogaine therapy.
Broader applications for neuropsychiatric conditions
The expanding research into ibogaine reveals promising applications beyond addiction treatment. The landmark $50 million Texas study, led by UTMB Health and UTHealth Houston, specifically focuses on ibogaine’s potential for treating traumatic brain injury, particularly in veterans suffering from PTSD and related conditions. This represents a significant expansion from ibogaine’s traditional use in addiction therapy centers.
The 2024 Stanford University study published in Nature Medicine has provided compelling evidence for ibogaine brain injury treatment, suggesting its effectiveness in addressing traumatic brain injuries—a leading cause of post-traumatic stress disorder. The Texas consortium’s research design includes dedicated focus areas, with UT Austin and Baylor College of Medicine concentrating specifically on traumatic brain injury applications in veterans, while other institutions examine addiction and associated behavioral health conditions.
This broader therapeutic potential positions ibogaine as a versatile psychedelic medicine capable of addressing multiple neuropsychiatric conditions simultaneously, offering hope for patients with complex, co-occurring disorders.
Path toward FDA approval and mainstream medical use
The path toward FDA approval represents the most significant milestone in ibogaine’s journey toward mainstream medical acceptance. The Texas consortium’s initiative marks the first major step toward obtaining FDA approval through rigorous clinical trials in the United States. This comprehensive approach includes partnerships with drug developers and teaching hospitals specifically designed to conduct FDA-approved clinical trials.
The collaborative effort will enable participating institutions to seek FDA approval for making ibogaine treatments more accessible while accelerating research and development. The Texas Health and Human Services Commission’s oversight ensures that all research meets the highest scientific and medical standards, with patient safety as the primary concern.
State legislation, including Senate Bill 2308, has provided the regulatory framework necessary for this advancement, authorizing $50 million in state-matching funds for clinical trials managed by public universities in partnership with pharmaceutical companies and hospitals. This legislative support demonstrates a commitment to evidence-based approaches in developing ibogaine for PTSD and other conditions.
The consortium’s comprehensive approach, combining expertise from multiple leading Texas institutions, positions the state at the forefront of ibogaine development for use in the United States, potentially establishing a model for national implementation.

Ibogaine represents a remarkable convergence of ancient wisdom and modern medicine, offering unprecedented hope for treating both addiction and traumatic brain injury. From its traditional use in Central African spiritual ceremonies to breakthrough clinical research showing 88% reductions in PTSD symptoms among military veterans, this powerful alkaloid demonstrates therapeutic potential unlike any other compound. The recent findings that ibogaine can restore cognitive function and dramatically improve quality of life for veterans with TBI mark a significant milestone in neuropsychiatric treatment.
As Texas invests $50 million in clinical trials and researchers develop safer analogues to address cardiotoxicity concerns, ibogaine’s journey toward FDA approval appears increasingly promising. However, the serious safety risks, including potential heart complications and complex drug interactions, underscore the critical importance of medical supervision and rigorous clinical oversight. For those struggling with treatment-resistant addiction or TBI, ibogaine may offer a path to recovery where other treatments have failed—but only under proper medical guidance and in appropriate clinical settings.
